A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Breast Reduction Surgery
Breast reduction surgery is also called reduction mammoplasty. Fat, tissue, and skin are removed from the breasts to make them smaller. The size of the dark skin around the nipple (areola) may be reduced. And the nipple may be moved higher on the breast.
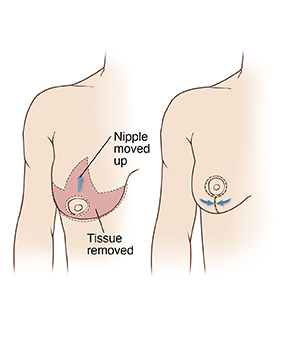 |
| This picture shows one method of breast reduction surgery. Talk to your surgeon about how your own surgery will be done. |
Getting ready for surgery
Prepare for the surgery as you have been told. Also:
-
Tell your -surgeon about any recent health conditions such as infections, and all medicines you take. This includes vitamins, herbs, and other supplements. It also includes any blood thinners, such as warfarin, clopidogrel, and certain anti-inflammatory medicines, such as daily aspirin. You may need to stop taking some or all of them before surgery.
-
Follow any directions you are given for not eating or drinking before surgery.
-
Don't smoke before or after surgery. Your healthcare provider may delay your surgery if you are smoking. Smoking reduces the blood flow in the skin and nipples, and increases the risk of wound healing problems. Nicotine from any source (cigarettes, e-cigarettes, patches, chewing tobacco) slows healing.
The day of surgery
The surgery takes about 2 to 4 hours. You may go home the same day. Or you may stay overnight in a hospital or outpatient surgical center.
Before the surgery begins
-
You will be asked to sign an informed consent form for both surgery and anesthesia. Be sure all of your questions about the procedure are answered before you sign.
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
You will be given medicine to keep you pain free during surgery. This may be general anesthesia, which puts you into a state like deep sleep. A tube may be put into your throat to help you breathe. Or you may have sedation, which makes you relaxed and sleepy. If you have sedation, local anesthesia will be injected to numb the area being worked on. The anesthesiologist will discuss your choices with you.
During the surgery
-
The healthcare provider makes 1 or more cuts (incisions) in your breast. Incisions are mostly made around the areola. But they extend down under your breast as well. You and your provider will have discussed incision sites before the surgery.
-
The healthcare provider removes fat, tissue, and skin from the breast. In some cases, fat is removed using liposuction. This means putting a hollow tube (cannula) into the breast. A special vacuum pulls fat through the cannula.
-
If needed, the areola and nipple are removed and positioned higher on the breast. To reduce the size of the areola, extra skin is removed. The areola is then stitched into place. The areola may be moved as a skin graft. This will result in a in a temporary or permanent loss of feeling in your nipples. Your healthcare provider will discuss which method is being used or is best for you.
-
The process is repeated on the other breast.
-
The incisions are closed with stitches, surgical glue, or both. A tube (drain) may be placed into the incisions before they are closed. This drains extra fluid as the wound starts to heal.
After the surgery
You will be watched as you wake up from the anesthesia. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. You will be given medicine to control pain or nausea. When you’re ready, you will be able to go home with an adult family member or friend. Or you may be moved to a room to stay overnight.
Recovering at home
Once you are home, follow any directions you are given. Your healthcare provider or surgeon will tell you when you can return to your normal routine. During your recovery:
-
Take any prescribed medicines exactly as directed.
-
Don't smoke or use nicotine products. These decrease blood flow and slows healing.
-
Wear the special bra or bandage you were given before discharge as directed by your surgeon or healthcare provider.
-
Care for your incisions and the dressing (bandage) over them as directed by your surgeon or provider.
-
Follow your surgeon or provider’s guidelines for showering. Don't swim, take a bath, use a hot tub, or do other activities that cause the incisions to be covered with water until your provider says it’s OK.
-
When you shower, gently wash your incision sites. Then pat the incisions dry. Don’t put lotions, oils, or creams on the incisions until after they are fully healed.
-
Don’t raise your arms above breast level for 10 days. And don’t lift, push, or pull anything heavier than 10 pounds for at least 7 days.
-
Don’t drive until you are no longer taking prescription pain medicine and your surgeon or healthcare provider says it’s OK. When riding in a car, carefully position the seatbelt so that it doesn’t go across your breasts.
-
Be aware that breast swelling may last for 3 to 5 weeks. Talk with your surgeon or provider about ways to manage the swelling. Follow directions as advised.
Call 911
Call 911 right away if you have:
-
Severe chest pain
-
Trouble breathing
When to call your healthcare provider
Call your healthcare provider if any of these occur:
-
A fever of 100.4° F ( 38°C ) or higher, or as advised by your provider
-
Bleeding or drainage through the special bra or bandage
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, pain that gets worse, or bad-smelling fluid leaking
-
Pain that is not eased by prescribed pain medicine or pain that gets worse
-
Much more soreness, swelling, or bruising on 1 breast than the other
-
Breast that is very warm to the touch
-
Symptoms get worse, or new symptoms occur
Follow-up
You will have follow-up visits so your surgeon or healthcare provider can see how well you’re healing. If needed, stitches or drains will be removed at one of these visits. If you have any questions or concerns about your recovery, let your healthcare provider know.
Risks and possible complications
Risks and possible complications include:
-
Bleeding or infection
-
Blood clots
-
Extra internal or external scarring
-
Breasts that are not the same shape or size
-
Breasts that are too firm
-
Changes in breast or nipple sensation (temporary or permanent)
-
Damage to nerves, muscles, or blood vessels
-
Open skin wounds
-
Pain that doesn't go away
-
Death of fat cells deep in the skin (fat necrosis)
-
Inability to breastfeed
-
Not happy with how your breasts look
-
Risks of anesthesia. The anesthesiologist will discuss these with you.
Online Medical Reviewer:
David Lickstein MD
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
2/1/2023
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.