A
B
C
D
E
F
G
H
I
J
K
L
M
N
O
P
Q
R
S
T
U
V
W
X
Y
Z
Click a letter to see a list of conditions beginning with that letter.
Click 'Topic Index' to return to the index for the current topic.
Click 'Library Index' to return to the listing of all topics.
Endoscopic Diagnosis of Chest, Lung Problems
Pulmonary endoscopy or bronchoscopy is a procedure for lung or airway-related symptoms such as persistent cough, coughing up blood, or difficulty breathing. This procedure lets your healthcare provider see the airway of your lungs and take a tissue sample (biopsy) or treat a lung condition if needed.
Bronchoscopy
A bronchoscopy lets the healthcare provider look into the airways in your lungs. This is done using a bronchoscope. A bronchoscope is a thin, flexible, hollow, lighted tube with a small camera that lets the healthcare provider see inside the lung. It's put through your nose or mouth, down your throat, and into your airways. Tools can be passed down the middle of the scope to collect tissue samples or remove any lumps or lesions.
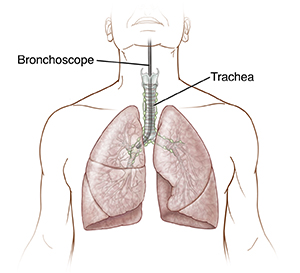 |
| With bronchoscopy, a flexible scope allows the healthcare provider to view and biopsy the airway. |
Transbronchial biopsy
This procedure is used mainly to take samples of tissue near the airway. It's done using a bronchoscope and tiny forceps. The forceps are passed through the scope into the airway, and a tissue sample is taken.
Endobronchial ultrasound
This is a type of bronchoscopy that looks at the lungs and the space between the lungs (mediastinum). This is done using a flexible bronchoscope and ultrasound. An ultrasound makes images using sound waves. These images guide the healthcare provider and let them see through the airway walls.
Getting ready for the procedure
Before your procedure, do the following:
-
Follow any directions you're given about not eating or drinking before the procedure.
-
Follow any other instructions from your healthcare provider. You may need to have blood tests. Follow any directions for not smoking.
-
Tell your provider about all the medicines you take. This includes over-the-counter and prescription medicines, vitamins, herbs, and other supplements. You may need to stop taking some of them before the procedure, especially aspirin, warfarin, or other blood thinners. Ask your provider what medicines to stop taking before the procedure.
-
Talk with your provider about any allergies and health problems you have.
-
Tell your provider if you're pregnant or think you could be pregnant.
-
Tell your provider if you're breastfeeding.
-
Ask your healthcare provider any questions you have about the procedure, risks, or recovery.
During the procedure
You'll get medicine through an IV (intravenous) line to help you relax and sleep during the procedure. You may also be given local anesthesia (numbing medicine) with a needle. Then a special spray is used to numb your throat and nose or mouth. This is to help keep you comfortable and prevent coughing during the procedure.
After the procedure
You will stay in the recovery room until the sedation wears off. This takes about 1 to 2 hours. Once you're fully awake, you can go home. You'll need an adult family member or friend to drive you home. You may have a cough, hoarse voice, or sore throat for 1 or 2 days. At first, there may be a small amount of blood in the saliva and mucus that you cough up (sputum). This is normal. It should go away after the second day.
Risks and possible complications
Possible risks include:
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
-
Large amounts of blood in sputum
-
Blood in sputum after 2 days
-
Shortness of breath
-
Chest pain
-
Fever of 100.4°F ( 38°C) or higher, or as directed by your healthcare provider
-
Hoarseness that won’t go away
-
Symptoms that get worse, or new symptoms
Online Medical Reviewer:
Chris Southard RN
Online Medical Reviewer:
Marianne Fraser MSN RN
Online Medical Reviewer:
Shaziya Allarakha MD
Date Last Reviewed:
3/1/2024
© 2000-2025 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.