Brown Syndrome
What is Brown syndrome in children?
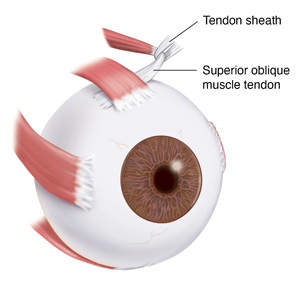
Brown syndrome is a problem with a tendon that attaches to the outside of the eye (superior oblique muscle tendon). In Brown syndrome, this tendon can't move freely. This limits the eye’s normal movements.
The superior oblique muscle is responsible for:
The superior oblique muscle tendon attaches to the superior oblique muscle. It moves through a ring of tissue. This is called the tendon sheath.
Many things can limit the normal movement of the muscle tendon through the tendon sheath. When that happens, Brown syndrome occurs.
Brown syndrome is a rare eye disorder. In most cases, a child is born with it (congenital). In very rare cases, it may happen later in life (acquired). Acquired Brown syndrome may be linked to other health conditions. These include injury, inflammatory diseases, problems from eye surgery, and sinus infection. It affects females more often than males.
What causes Brown syndrome in a child?
Problems with how the superior oblique muscle tendon or its sheath are formed can cause symptoms of Brown syndrome. The muscle tendon or its sheath might be abnormally short or thick from birth. Some cases of Brown syndrome might be partly due to problems in the genetic information passed from parents to children. Experts don't yet know what genes might be affected. Most children born with Brown syndrome have no family history of the disease.
Which children are at risk for Brown syndrome?
At least some cases of Brown syndrome tend to run in families. Your child may be at greater risk for Brown syndrome if someone in your family has it. You might also be at greater risk if you have any health conditions that can cause it, such as lupus. Getting treatment for your health condition right away may help reduce your risk of getting Brown syndrome.
What are the symptoms of Brown syndrome in a child?
In most cases, only one eye is affected. This is most often the right eye. But both eyes can be affected. The symptoms can vary in severity.
Brown syndrome limits the normal movements of the eye. For example:
-
If Brown syndrome affects the right eye, your child may not be able to look up with the right eye when their eyes are looking to the left. It may cause mild pain when your child tries to make this eye movement.
-
If Brown syndrome affects the left eye, your child may not be able to look up with the left eye when their eyes are looking to the right. The eyes might look normal when looking toward the midline or straight ahead. The affected eye might be a bit lower than the other eye.
Other symptoms include:
If these problems are present from birth, they are often constant. But they may slowly get better.
How is Brown syndrome diagnosed in a child?
Diagnosis begins with a health history and physical exam. This includes a full eye exam. Young children can't really follow the directions of a normal eye exam. So healthcare providers can find it hard to diagnose Brown syndrome in young children. You may need an experienced eye care provider to make the diagnosis for your child.
Your child may need imaging tests to get more information about the superior oblique muscle tendon.
How is Brown syndrome treated in a child?
Treatment will depend on your child's symptoms, age, and general health. It will also depend on how severe the condition is. And on what is causing it.
Close watching often works in mild cases.
More severe cases of Brown syndrome may need surgery. Your child may be more likely to need surgery if:
-
The eyes are out of alignment when looking straight ahead
-
Your child has double vision
-
The head position is abnormal
During this surgery, the eye surgeon may cut the superior oblique muscle tendon and use a device to lengthen it. This may allow the muscle tendon to move normally. The surgery is often successful. But some children need repeat surgery.
Brown syndrome due to other conditions is more likely to go away without surgery. Treating the underlying health condition may help reduce symptoms. For example, someone with Brown syndrome due to lupus might find it helpful to be treated with corticosteroids.
When should I call my child's healthcare provider?
If your child has Brown syndrome, watch their symptoms closely. Your child will need close follow-up care. If symptoms get worse, plan to see your child's eye care provider soon. Your child might need surgery.
Key points about Brown syndrome in children
-
Brown syndrome is a rare problem with a muscle tendon on the outside of the eye. The tendon can't move freely. The eye's normal movement is limited.
-
In most cases, this condition is present from birth. In very rare cases, it occurs later in life.
-
It often affects only one eye. But both eyes can be affected.
-
Your child may have trouble looking to the opposite side, and upward, with the affected eye.
-
If your child has a mild case, close observation may be advised.
-
In more severe cases, children may need surgery.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
-
Know the reason for the visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
-
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
-
Ask if your child’s condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if your child does not take the medicine or have the test or procedure.
-
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.